
Moreover, complications directly related to intubation and mechanical ventilation can be avoided, such as aspiration, trauma to surrounding structures, barotrauma, ventilator-associated pneumonia. 3 Compared with invasive ventilation, NIV is more comfortable while preserving the patient's airway defense mechanism. 2 Invasive methods bypass the upper airway and include options such as an endotracheal tube, a laryngeal mask, or a tracheostomy. NIV has gained more popularity as it provides ventilation to the patient without using an artificial airway and does not bypass the upper airway.

Providing supplemental oxygen, whereas relatively free of complications, through noninvasive oxygenation and ventilation modalities are helpful as one investigates the underlying etiology for the patient’s hypoxemia.

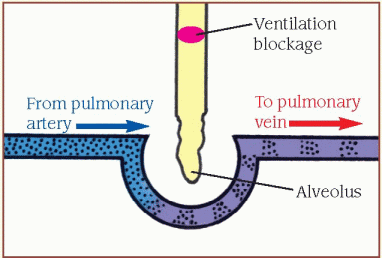
As mentioned before, there are numerous reasons why a patient may become hypoxemic, including subambient Fi02, hypoventilation, V/Q mismatch, shunt, or diffusion defects which can manifests clinically as tachycardia, arrhythmias, feeling short of breath, dyspnea, tachypnea, altered mental status, and use of accessory muscles and indicate the need for supplemental oxygen.
In adults, hypoxemia is commonly defined as a Pa o 2 less than 80 mm Hg on room air at sea level. This article will review some essential noninvasive oxygenation and ventilation strategies most commonly used in the surgical arena, hoping that it will provide a good reference when deciding which modality to choose in a hypoxic patient. The ability to understand and use different noninvasive ventilation (NIV) modalities is a valuable tool to have in your armamentarium before transitioning to more invasive strategies. It is not an uncommon clinical scenario in medicine and surgery whereby one encounters a hypoxemic patient due to a myriad of reasons.


 0 kommentar(er)
0 kommentar(er)
